Global and Regional Cardiovascular Mortality Attributable to Nonoptimal Temperatures Over Time
Abstract
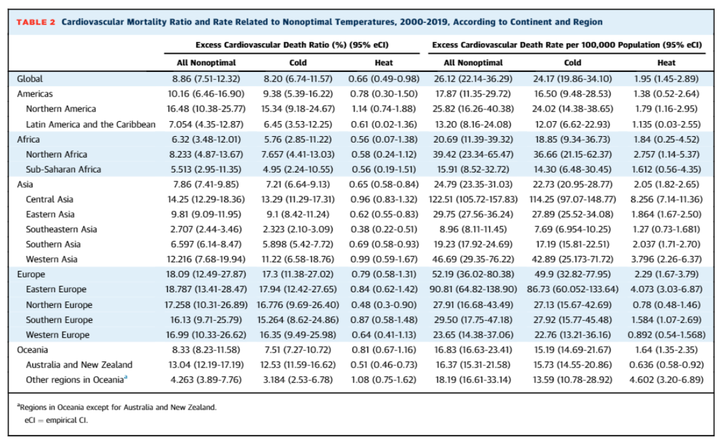
Background. The association between nonoptimal temperatures and cardiovascular mortality risk is recognized. However, a comprehensive global assessment of this burden is lacking. Objectives. The goal of this study was to assess global cardiovascular mortality burden attributable to nonoptimal temperatures and investigate spatiotemporal trends. Methods. Using daily cardiovascular deaths and temperature data from 32 countries, a 3-stage analytical approach was applied. First, location-specific temperature–mortality associations were estimated, considering nonlinearity and delayed effects. Second, a multivariate meta-regression model was developed between location-specific effect estimates and 5 meta-predictors. Third, cardiovascular deaths associated with nonoptimal, cold, and hot temperatures for each global grid (55 km × 55 km resolution) were estimated, and temporal trends from 2000 to 2019 were explored. Results. Globally, 1,801,513 (95% empirical CI: 1,526,632-2,202,831) annual cardiovascular deaths were associated with nonoptimal temperatures, constituting 8.86% (95% empirical CI: 7.51%-12.32%) of total cardiovascular mortality corresponding to 26 deaths per 100,000 population. Cold-related deaths accounted for 8.20% (95% empirical CI: 6.74%-11.57%), whereas heat-related deaths accounted for 0.66% (95% empirical CI: 0.49%-0.98%). The mortality burden varied significantly across regions, with the highest excess mortality rates observed in Central Asia and Eastern Europe. From 2000 to 2019, cold-related excess death ratios decreased, while heat-related ratios increased, resulting in an overall decline in temperature-related deaths. Southeastern Asia, Sub-Saharan Africa, and Oceania observed the greatest reduction, while Southern Asia experienced an increase. The Americas and several regions in Asia and Europe displayed fluctuating temporal patterns. Conclusions. Nonoptimal temperatures substantially contribute to cardiovascular mortality, with heterogeneous spatiotemporal patterns. Effective mitigation and adaptation strategies are crucial, especially given the increasing heat-related cardiovascular deaths amid climate change.